Authors: Charles A. Nelson & Lauren Baczewski
Participating in standard cognitive testing can be challenging for those with Rett Syndrome (RTT) due to the disorder’s impact on language and motor skills. For example, many classic intelligence tests require individuals to select their answers using spoken words and/or by pointing. These requirements for selecting an answer prevent many from participating and present obstacles in accurately assessing the individual’s intellectual functioning. For the past few years, with generous funding from IRSF, our team in the Labs of Cognitive Neuroscience at Boston Children’s Hospital has embarked on an ambitious program of research to adapt a cognitive assessment (the Mullen Scales for Early Learning) for use with children with RTT. Our goal is to minimize verbal and motor requirements to obtain a more objective reading of the child’s cognitive ability by adapting the assessment to be administered on an eye tracking computer. In doing so, we rely on the child’s ability to engage in coordinated eye movements to illustrate their answer to each question.
The Mullen Scales of Early Learning (MSEL) is a developmental cognitive assessment used with children from early infancy to5 ½ years of age. This play-based, interactive assessment includes 5 domains or “scales” including fine motor, gross motor, expressive language, receptive language, and visual reception. The examiner sits across from the child and presents her with a series of objects and pictures while asking questions. As we outline in our first published paper (Clarkson et al., in press), we have adapted the MSEL in two ways. First, with permission from Pearson Inc., we employed various strategies to develop what we call the “Adapted MSEL.” In this variation on the conventional assessment, we wait longer for responses, use hand-bracing when helpful, and accept broad swipes, taps, or directed eye gaze in place of pointing to answer questions. We compared the scores of 47 girls with RTT to normative scores in each domain of the MSEL. Scores in the fine motor and expressive language domains were at, or consistently below 50%, which is to be expected given that the diagnostic symptoms of RTT include impaired verbal communication and loss of purposeful hand movements. However, we were encouraged to find that visual reception and receptive language performance varied from “very low” to “very high” across individuals with RTT.
Findings indicate that some girls with RTT are able to perform at or even above their age level when they are tested in ways that do not rely on verbal responses or fine motor skills.Indeed, one 30-month-old girl scored “very low” (14-month equivalent) in fine motor and “very low” (8-month equivalent) in expressive language, but “average” (34-month equivalent) in receptive language and “very high” (48-month equivalent) in visual reception. This incredible case should encourage caregivers and teachers to intellectually challenge girls with RTT to maximize their potential.
In order to obtain a more objective reading of our children’s eye gaze-directed responses, we next adapted the MSEL for use with a Tobii (©) eye tracker. As many parents and clinicians are aware, Tobii eye trackers are increasingly being used to help children communicate. We therefore took advantage of this familiarity by adapting a subset of the items on the MSEL for use with our Tobii. Specifically, we presented images of the exact objects and items used in the traditional MSEL assessment on the Tobii platform. Before presenting each item to the child, we calibrated their eyes to the Tobii screen to ensure that the computer was accurately capturing their gaze. As each question was presented, we used the live viewer function in Tobii studio to reflect the participant’s eye gaze, so that they could see their gaze on the screen at all times (gaze is represented as the red dot as seen below in Figure 1). We then introduced the task to the child and asked them look at their answer. Figure 1 illustrates an example of a matching task from the MSEL, including a participant’s gaze as depicted in red.
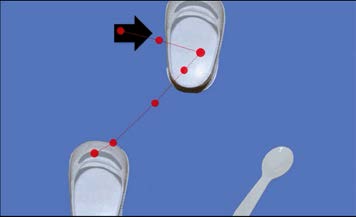
Figure 1: When presented with the 3 items shown, the child is asked to look at the one that looks like the target object (indicated by the black arrow).
We have administered the finalized version of the eye tracking MSEL to 27 children with RTT and 32 typically developing children of similar chronological ages. This comparison allows us to collect normative data and receive feedback from a verbal population as to improvements that can be made to continually modify this instrument.
Conclusions
We are very optimistic about the progress we have made thus far. There are two challenges that lie ahead, however. The first is to collect normative data on a larger sample of typically developing participants to complete both a standard MSEL and eye tracking MSEL. We will then be able to compare scores for each participant on the two measures and further determine the validity of the eye tracking adaptation. The second is to expand the number of subtests on the original MSEL that can be used with eye tracking. The challenge here, of course, is that evaluating expressive language, fine and gross motor skills could prove daunting.
For more information on our ongoing Rett syndrome and related disorders research please visit:
http://www.childrenshospital.org/research-and-innovation/research/labs/laboratories-of-cognitive-neuroscience/current-research-projects/rett-syndrome
Reference
Clarkson, T. LeBlanc, J., Degregorio, G., Vogel-Farley, V., Barnes, K., Kaufmann, W.E., Nelson, C.A. (in press). Adapting the Mullen Scales of Early Learning for a Standardized Measure of Cognition in Children with Rett Syndrome. American Journal on Intellectual and Developmental Disabilities.
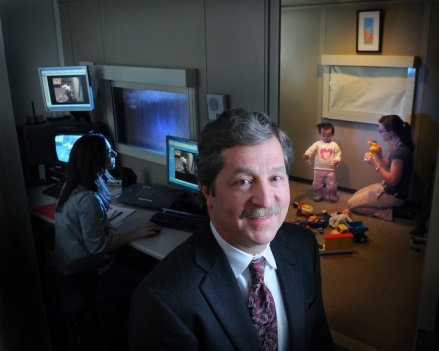 Charles A. Nelson III, PhD, is Professor of Pediatrics and Neuroscience and Professor of Psychology in the Department of Psychiatry at Harvard Medical School, and holds the Richard David Scott Chair in Pediatric Developmental Medicine Research at Boston Children’s Hospital. His research interests center on a variety of problems in developmental cognitive neuroscience, including: typical and atypical memory development; the development of social perception; developmental trajectories to autism; and the effects of early adversity on brain and behavioral development.
Charles A. Nelson III, PhD, is Professor of Pediatrics and Neuroscience and Professor of Psychology in the Department of Psychiatry at Harvard Medical School, and holds the Richard David Scott Chair in Pediatric Developmental Medicine Research at Boston Children’s Hospital. His research interests center on a variety of problems in developmental cognitive neuroscience, including: typical and atypical memory development; the development of social perception; developmental trajectories to autism; and the effects of early adversity on brain and behavioral development.
 Lauren Baczewski, M.A., is the Clinical Research Coordinator for all rare genetic disorder projects in the Nelson Lab at Boston Children’s Hospital. Her research interests include early markers of risk for atypical development and the development of family-focused interventions for children with neurodevelopmental disorders, particularly children with autism and related genetic disorders. She has worked extensively with individuals with Rett Syndrome as a behavioral interventionist and in the context of clinical research. She will attend UCLA in the fall to pursue a PhD in Human Development & Psychology.
Lauren Baczewski, M.A., is the Clinical Research Coordinator for all rare genetic disorder projects in the Nelson Lab at Boston Children’s Hospital. Her research interests include early markers of risk for atypical development and the development of family-focused interventions for children with neurodevelopmental disorders, particularly children with autism and related genetic disorders. She has worked extensively with individuals with Rett Syndrome as a behavioral interventionist and in the context of clinical research. She will attend UCLA in the fall to pursue a PhD in Human Development & Psychology.